Pediatric GI Treatment and Services

Get care for your child’s gastrointestinal disease at OHSU
For a child with digestive symptoms, finding the cause is the first step. Work with our team to test, diagnose and treat your child’s gastrointestinal (GI) condition so they feel better and get back to their normal daily life.
How to find care at Doernbecher
Please contact us to request an appointment or ask questions.
Call 503-494-1078
Conditions we treat
Services and procedures
Aerodigestive disorders
What are pediatric aerodigestive disorders?
An aerodigestive disorder is a combination of conditions that affect your child’s breathing, swallowing or growth. It occurs when they get food or liquid in their lungs or airways, making it hard to breathe or swallow.
Treatment for aerodigestive disorders
If your child has an aerodigestive disorder, your pediatrician may refer you to our pediatric gastroenterology team. We collaborate with Doernbecher’s aerodigestive care team to treat children with complex symptoms, such as aspiration, chronic cough and airway obstruction, that impact breathing and digestion. Your child’s care may include medication, surgery, nutrition and other approaches.
Meet our team
-
- Henry Lin, M.D., M.B.A.
- Accepting new patients
Constipation and encopresis
What is constipation?
Constipation is infrequent bowel movements or hard, dry stools that are hard to pass. Most pediatric constipation is easy to treat at home or through a pediatrician.
What is encopresis?
Encopresis, or fecal incontinence, is when children over age 4 pass stools into places other than the toilet (like their underwear or on the floor). It often includes constipation. Our specialized encopresis clinic treats children ages 4 to 16 with encopresis.
Treatment for constipation and encopresis
We use medical and behavioral methods to manage constipation and encopresis in children. If your child has chronic or severe constipation or encopresis, your pediatrician may refer you to us. A gastroenterology nurse practitioner and a psychologist work with your child to create a treatment plan, which may include:
- Laxatives or other medications for bowel management.
- Support for toilet behaviors, such as sitting on the toilet, stooling into the toilet or cleaning up when soiled.
-
- Chelsea Doherty, M.S.N., RN, CPNP
- Accepting new patients
-
- Ruth Duffield, M.S.N., FNP, CWOCN
- Accepting new patients
-
- Suzanne Kavet, M.S.N., RN, CPNP-C
- Accepting new patients
-
- Christina Low Kapalu, Ph.D. (she/her)
- Accepting new patients
Cystic fibrosis
What is pediatric cystic fibrosis?
Cystic fibrosis is a genetic disease that affects the lungs and digestive system. Children with cystic fibrosis may have lung infections, malnutrition and other complications.
Treatment for pediatric cystic fibrosis
Our pediatric gastroenterology specialists collaborate with Doernbecher’s cystic fibrosis care team to treat children with cystic fibrosis. You will find:
- World-class pediatric cystic fibrosis specialists
- Complete care for your child, including diagnosis, treatment, medication and monitoring
- Oregon’s only nationally accredited Cystic Fibrosis Care Center staffed by pediatric pulmonologists
Hillary Bashaw, M.D., pediatric gastroenterologist
-
- Kimberly Trieschmann, M.D.
- Accepting new patients
Eosinophilic esophagitis
What is eosinophilic esophagitis?
Eosinophilic esophagitis is an auto-immune disease that causes white blood cells (eosinophil) to build up in the esophagus, or throat. The built-up blood cells can make it hard to eat or swallow and can damage the esophagus. Food or other allergies, or acid reflux may trigger symptoms.
Treatment for eosinophilic esophagitis
Our GI physicians, dietitians, psychologists and allergy specialists work together to care for your child’s eosinophilic esophagitis symptoms. Treatment may include eliminating food, taking medication every day or managing injections. Your child may see a dietitian, feeding specialist, GI psychologist and allergist as part of their treatment plan.
-
- Emily Whitfield, M.D., M.Sc. (she/her)
- Accepting new patients
Gut-brain interaction disorders and IBS
What are disorders of the gut-brain interaction?
These conditions occur when the gut and brain interaction, or gut-brain connection, isn’t working right.
The gut-brain connection is the evidence-based link between the brain and digestive health. For example, digestive issues may send signals to the brain and central nervous system that affect thinking, memory and emotions.
What is irritable bowel syndrome (IBS)?
IBS is one of the most common gut-brain disorders. Symptoms of IBS may include abdominal pain, bloating, acid reflux, nausea and feeling full quickly.
Treatment for gut-brain interaction disorders and IBS
Gut-brain disorder symptoms are hard to treat with medication alone. Research shows that learning to understand the gut-brain connection makes a difference.
Our integrative gut health program teaches your child about the connection between the gut and brain. We care for children with gut-brain interaction disorders (previously called functional GI disorders), including IBS. Your child’s gastroenterologist may refer you to our program.
Your child may see a gastroenterologist and a psychologist who can help:
- Identify triggers for GI symptoms, like pain or nausea.
- Manage GI symptoms with effective, research-based strategies.
- Learn how stress, anxiety, sleep, exercise and nutrition affect gut health.
Resources for pediatric gut-brain interaction and IBS
- Children and functional GI problems: An overview from the Canadian Society of Intestinal Research
- Pediatric and adolescent functional GI disorders: An overview from the American College of Gastroenterology
- The brain-gut connection, explained: An overview from OHSU specialists
- Understanding pediatric chronic abdominal pain
-
- Amanda Lee, M.D., M.Ed.
- Accepting new patients
Polyposis syndromes
What are polyposis syndromes?
In polyposis syndromes, polyps or small growths build up in the colon or GI tract. These diseases are hereditary. Polyposis syndromes found in children include:
- Familial adenomatous polyposis
- Peutz-Jeghers syndrome
- Juvenile polyposis syndrome
- Serrated polyposis syndrome
- Cowden syndrome (also known as PTEN hamartoma tumor syndrome)
Treatment for polyposis syndromes in kids
Our polyposis team of experts treats children with confirmed or suspected polyposis conditions. A gastroenterologist, psychologist and genetic counselor specializing in pediatric polyposis will work with you and your child to create a treatment plan.
- A gastroenterologist evaluates and treats your child’s condition.
- A psychologist supports your child’s quality of life.
- A genetic counselor answers questions about genetic testing, comorbidities and genetic risks for polyposis syndromes in other family members.
-
- Henry Lin, M.D., M.B.A.
- Accepting new patients
-
- Christina Low Kapalu, Ph.D. (she/her)
- Accepting new patients
-
- Kelly Jo Hamman, M.S., CGC
- Accepting new patients
Ariel Porto, M.D., pediatric gastroenterologist
Short gut syndrome
What is short gut syndrome?
Short gut syndrome, also called short bowl syndrome (SBS), is when a child’s small intestine is too short. Some children with short gut syndrome can’t absorb enough nutrients from the food they eat.
Treatment for short gut syndrome
We provide complete care and intestinal rehabilitation to help children with short gut syndrome or intestinal failure. Treatment may include:
- Malabsorption treatment to replace missing nutrients
- Nutrition
- Feeding
- Medication
- Surgery
- Psychological support
In rare cases, your child might need a bowel transplant. We will work closely with a pediatric transplant center at another hospital in our region to get them the best possible care.
Your child’s care team may include a gastroenterologist, GI psychologist, dietitian, feeding specialist, pharmacist, social worker, nurse coordinator and surgeon. You’ll find help to:
- Manage your child’s medications.
- Learn more about their condition.
- Schedule appointments with our team.
- Work with your insurance carrier to get medicines and tests approved.
-
- Mikelle D. Bassett, M.D.
- Accepting new patients
Hillary Bashaw, M.D., pediatric gastroenterologist
Brittany Cummiskey, pharmacist
Psychology services
Working with a psychologist can help kids manage their GI health conditions. This does not mean your child has a mental health disorder.
How do psychologists treat GI diseases?
Our psychologists are experts in supporting children with GI conditions. They use evidence-based cognitive and behavioral care to address mental, physical, social and cultural factors that impact GI diseases and symptoms. GI psychologists help kids:
- Manage GI symptoms, like abdominal pain and nausea.
- Cope with a chronic illness.
- Navigate school, friends, family, sports and other activities when they have chronic GI symptoms.
Your child’s care team may include a psychologist if they are referred by a gastroenterologist or if they are part of one of these programs:
- Celiac disease
- Constipation and encopresis
- Eosinophilic esophagitis
- Gut-brain interaction disorders and IBS
- Inflammatory bowel disease (IBD)
- Liver diseases
- Polyposis syndromes
-
- Christina Low Kapalu, Ph.D. (she/her)
- Accepting new patients
Transitioning to adult care services
Many GI diseases and conditions are lifelong. As your child becomes a young adult, we will support and prepare them to transition to an adult GI care team.
How will you help my child transition to adult GI care?
Adult care doesn’t necessarily start when your child turns 18. We consider their age, condition, preferences and current treatments as we work with your family to make the transition.
Your child will learn to take responsibility for their health care as they enter adolescence and adulthood. We help them:
- Feel comfortable talking independently with their providers.
- Know their medications, side effects and personal medical history.
- Manage their medications and refill prescriptions.
- Understand medical bills and insurance plans.
- Feel secure managing their condition in new environments, like college and work.
- Know what resources and tools are available to them.
- Choose their new care setting and share their health history with their new providers.
We also support parents and caregivers and offer workshops to help families transfer health care responsibilities to their teens.
Resources for transitioning to adult care
Improve Care Now: Toolkit for the transition to adult care
Tests to diagnose and treat GI conditions
Gastrointestinal (GI) diseases and conditions have many symptoms in common. Doctors use tests and procedures to diagnose and treat GI disorders in children. They look for a range of causes, including genetic food allergies, stomach acid, polyps, blockages, bacteria and more.
Here are common GI tests and procedures we provide at Doernbecher.
Anorectal manometry
We place a small tube with a balloon at the tip into the rectum. Sensors on the tube measure pressure and response of the anal sphincter and rectal muscles. This test helps us evaluate children with constipation or fecal incontinence.
Bravo esophageal pH test
During endoscopy, we place a wireless pH probe in the esophagus. Over the next few days, the probe will measure how much stomach acid is leaving your child’s stomach. The probe will naturally pass from your child’s body in a bowel movement.
Breath test
Your child will drink a special liquid and wear a nasal breathing tube. Over an hour, we will measure levels of certain gases or bacteria in their breath. This non-invasive test helps us diagnose lactose or fructose intolerance, or overgrowth of bacteria.
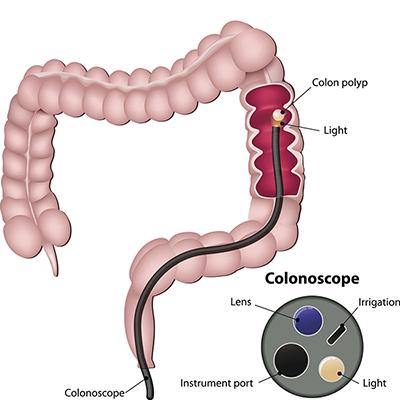
Colonoscopy
We place a thin tube with a camera at the end through the rectum. This test lets us look for inflammation and polyps in your child’s large intestine (colon). Your child will be asleep during the procedure.
Endoscopy
What is endoscopy?
Endoscopy is a procedure to see inside the body using a long thin tube with a camera at the end. Doctors may choose endoscopy to examine, diagnose and sometimes treat your child’s condition.
To see the esophagus, stomach and duodenum, we place the endoscopic tube through the nose or mouth. We can look for inflammation and test motility (movement processes). Your child will be asleep during the procedure.
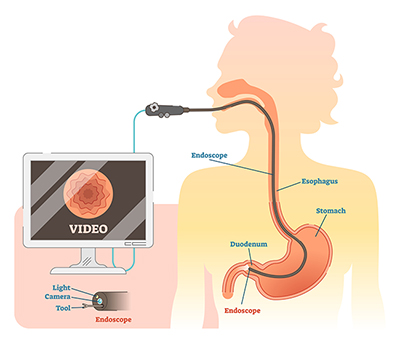
What are the types of endoscopies?
There are many types of endoscopic procedures, but they work about the same. The name usually refers to an area of the body. For example, a colonoscopy is an endoscopy for the colon.
Capsule endoscopy
If we need to see your child’s small intestine or full digestive system, we may recommend a capsule endoscopy procedure. Your child swallows a capsule with a tiny camera inside. As it moves through their digestive system, it takes thousands of pictures.
Gastro-jejunal feeding tube (GJ-tube) conversion
Most children with feeding tubes start with a G-tube. If your child still has symptoms like reflux or vomiting, we can replace the G-tube with a GJ-tube. This tube extends through the stomach into the jejunum (small intestine). The G-tube is removed and GJ-tube placed in the same procedure. Your child will be asleep throughout.
Gastrostomy feeding tube (G-tube) placement
We place a thin tube with a camera at the end through the nose or mouth (endoscopy) to help guide the g-tube placement. We make a small cut in the left side of the abdomen and insert a flexible, hollow tube (the G-tube) into the stomach. Your child will be asleep during the procedure.
pH/impedance probe
We place a thin tube through the mouth into the esophagus. A sensor on the end of the tube will measure how much stomach acid is leaving your child’s stomach.
Therapeutic and advanced endoscopy
These procedures can both diagnose and treat certain conditions. They are often less invasive and more effective than a simple endoscopy. We are the only program in the Pacific Northwest offering advanced endoscopy for children.
If your child has a complex GI condition, such as pancreatic disease or obstructive gallstones, they may need advanced endoscopy as part of their treatment. These may include:
- Endoscopic retrograde pancreatography
- Endoscopic ultrasound
- Double balloon enteroscopy
How does therapeutic endoscopy treatment work?
Gastroenterologists meet with you and your family to discuss your child’s condition and the type of endoscopy they need. You will learn more about the procedures and create a treatment plan for your child.
-
- Henry Lin, M.D., M.B.A.
- Accepting new patients
-
- Saad Jazrawi, M.D.
- Accepting new patients
Ariel Porto, M.D., pediatric gastroenterologist
Resources for patients and families
- GIkids: Details on pediatric GI conditions, including symptoms, treatments and more.
- Rood Family Pavilion: A home away from home for families who need to travel to Doernbecher for medical care.
- Doernbecher amenities: Family lounges, play areas, resource center and more.
- Child life specialists: Support for all the children in your family, not just patients.
- Animal-assisted therapy: Certified therapy dogs provide comfort to kids who need to stay in the hospital.
- Social workers: Emotional and social support for your child and family, including financial resources, transportation, housing and more.
- Hospital school program: Professional teachers keep children learning while they are in the hospital.
- Spiritual services: Support for people of all faiths to cope with the challenges that may come up when a child is sick.
- Palliative care: Programs to help children with serious conditions live full and meaningful lives, even when the future is uncertain.
Locations
Parking is free for patients and their visitors.
Doernbecher Children’s Hospital
700 S.W. Campus Drive
Portland, OR 97239
Map and directions
Find other locations across Oregon and in southwest Washington.
For providers
- Refer a patient to Doernbecher.
- Call for provider advice: 503-346-0644
- Fax patient records and lab work: 503-418-1377
Medical treatment guides
- Constipation
- Functional abdominal pain
- Fatty liver (NAFLD)
- Work-up needs before your patient visits us
- Colonoscopy prep for your patients